Cervical cancer is cancer that starts in the cervix, the lower, narrow part of the uterus (womb). Most cervical cancers are caused by the human papillomavirus (HPV). Cervical cancer is the easiest gynecological cancer to prevent with regular screening tests and vaccination. It is also very curable when found and treated early.
What is cervical cancer?
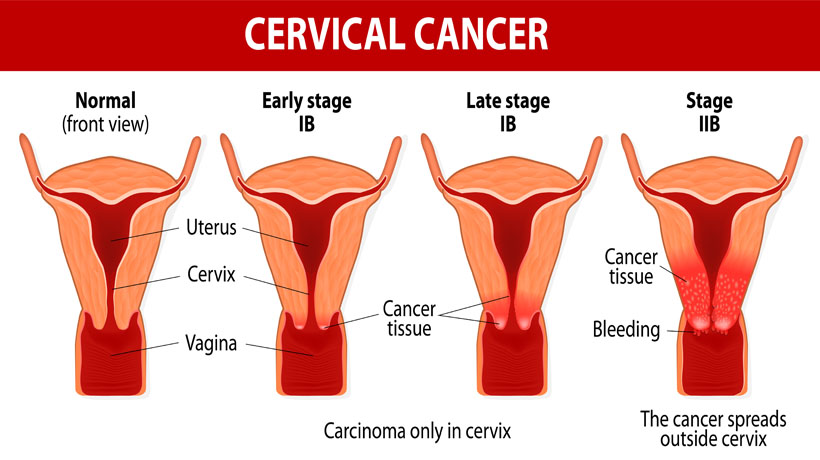
Cervical cancer is cancer that starts in the cervix, the lower, narrow part of the uterus. It happens when the body’s cervical cells divide very fast and grow out of control. These extra cells form a tumor.
Who gets cervical cancer?
Each year, about 12,000 women in the United States get cervical cancer. Cervical cancer happens most often in women 30 years or older, but all women are at risk.
What causes cervical cancer?
Most cases of cervical cancer are caused by a high-risk type of HPV. HPV is a virus that is passed from person to person through genital contact, such as vaginal, anal, or oral sex. If the HPV infection does not go away on its own, it may cause cervical cancer over time.
Other things may increase the risk of developing cancer following a high-risk HPV infection. These other things include:
- Smoking
- Having HIV or reduced immunity
- Taking birth control pills for a long time (more than 5 years)
- Having given birth to three or more children
What are the symptoms of cervical cancer?
You may not notice any signs or symptoms of cervical cancer. Signs of advanced cervical cancer may include bleeding or discharge from the vagina. These symptoms may not be caused by cervical cancer, but the only way to be sure is to see your doctor.
How do I find out if I have cervical cancer?
Women should start getting screened at age 21. You can get a Pap test to look for changes in cervical cells that could become cancerous if not treated. If the Pap test finds major changes in the cells of the cervix, your doctor may suggest more tests to look for cancer. Women between the ages of 30 and 65 can also get an HPV test with your Pap test to see if you have HPV.
What is the difference between a Pap test and an HPV test?
The Pap test and the HPV test look for different things.
A Pap test checks the cervix for abnormal cell changes that, if not found and treated, can lead to cervical cancer. Your doctor takes cells from your cervix to examine under a microscope. How often you need a Pap test depends on your age and health history. Talk with your doctor about what is best for you.
An HPV test looks for HPV on a woman’s cervix. Certain types of HPV can lead to cervical cancer. Your doctor will swab the cervix for cells. An HPV test is not the same as the HPV vaccine.
According to the U.S. Preventive Services Task Force (USPSTF), women ages 30 to 65 can combine the HPV test with a Pap test every 5 years. The USPSTF does not recommend the HPV test for women under age 30.
How often do I need to be screened for cervical cancer?
How often you need to be screened depends on your age and health history. Talk with your doctor about what is best for you. Most women can follow these guidelines:
- If you are between ages 21 and 29, you should get a Pap test every 3 years.
- If you are between ages 30 and 64, you should get a Pap test and HPV test together every 5 years or a Pap test alone every 3 years.
- If you are 65 or older, ask your doctor if you can stop having Pap tests.
If you had a hysterectomy, you should follow these guidelines:
- If you no longer have a cervix because you had a hysterectomy for reasons other than cancer, you do not need Pap tests.
- If you had a hysterectomy because of abnormal cervical cells or cervical cancer, you should have a yearly Pap test until you have three normal tests.
- If you had your uterus removed but you still have a cervix (this type of hysterectomy is not common), you need regular Pap tests until you are 65 and have had three normal Pap tests in a row with no abnormal results in the last 10 years.
How can I lower my chances of getting cervical cancer?
You can lower your chances of getting cervical cancer in several ways:
- Get regular Pap tests. Regular Pap tests help your doctor find cell changes and treat any unhealthy cells before they turn into cancer.
- Get regular Pap and HPV tests together or an HPV test alone (if you are between 30 and 65 years old).Doctors recommend getting an HPV test or co-testing (getting a Pap and HPV test together) for most women between 30 and 65.
- Get the HPV vaccine. Cervical cancer is usually caused by types of HPV that are passed from person to person through genital contact. Most women do not have symptoms of HPV, and HPV sometimes goes away on its own. If HPV does not go away on its own, it can cause changes in the cells of the cervix that can lead to cervical cancer. The HPV vaccine prevents you from getting most cancer-causing types of HPV. The Food and Drug Administration (FDA) approved the HPV vaccine for people ages 9 through 45.
- Take steps to lower your risk. If you have sex, lower your risk of getting HPV with the following steps:
- Use condoms. Condoms are the best way to prevent STIs when you have sex. HPV can happen in female and male genital areas that are not protected by condoms. But research shows that condom use is linked to lower cervical cancer rates.1,2 Also, the HPV vaccine does not replace or decrease the need to wear condoms. Make sure to put the condom on before the penis touches the vagina, mouth, or anus. Other methods of birth control, like birth control pills, shots, implants, or diaphragms, will not protect you from HPV or other STIs.
- Get tested. Be sure you and your partner are tested for STIs. Talk to each other about the test results before you have sex.
- Be monogamous. Having sex with only one partner can lower your risk of STIs. After being tested for STIs, be faithful to each other. That means that you have sex only with each other and no one else.
- Limit your number of sex partners. Your risk of getting STIs goes up with the number of sexual partners you have.
- Do not douche. Douching removes some of the normal bacteria in the vagina that protect you from infection. This may increase your risk of getting STIs.
- Be aware of how much alcohol you drink and keep control of your own drink. Some people use alcohol or drugs as a way to make a person drunk or high. Someone who is drunk, drugged, or high on drugs is unable to consent or understand what is ha
Who should get the HPV vaccine?
Experts recommend that most people get the HPV vaccine at age 11 or 12. The HPV vaccine works best when you get it before you have any type of sexual contact with someone else. The Food and Drug Administration (FDA) approved the HPV vaccine for people ages 9 through 45. There is not enough research to show whether the HPV vaccine is safe during pregnancy. As a result, experts do not recommend the HPV vaccine for pregnant women.
If you are 45 or younger and never had the HPV vaccine, or did not get all of the HPV shots, ask your doctor or nurse about getting vaccinated.
Do I need the HPV vaccine if I have already had sexual contact?
Yes. You can still benefit from the HPV vaccine if you have already had sexual contact with someone else. The vaccine can protect you from HPV types you haven’t gotten yet.